Telemedicine App Development: Features, Costs and Planning
- A brief about telemedicine app development
- The Market Health of Telemedicine apps
- How to develop a telemedicine application?
- 1. Research and Planning
- 2. Choosing a Business Model
- 3. Define Features
- 4. Design the User Interface (UI)
- 5. Develop the Backend
- 6. Implement Security and Compliance
- 7. Testing and Quality Assurance
- 8. Launch and Gather Feedback
- 9. Maintenance and Updates
- 10. Marketing and Scaling
- How much does a telemedicine application cost?
- Type of Telemedicine App
- Design Costs
- Development Costs
- Features and Functionality
- Third-Party Integrations
- Compliance and Security
- Quality Assurance (QA) & Testing
- Post-Launch Maintenance and Support
- Cloud Infrastructure and Hosting
- Marketing and Launch Costs
- What are different monetization models of tele-medicine applications?
- Essential features that a telemedicine MVP should have
- Essential features that a full-fledged application should have
- Breaking Down the Types of Telemedicine applications
- Real-time Telemedicine (Synchronous Telemedicine)
- Store-and-Forward Telemedicine (Asynchronous Telemedicine)
- Remote Patient Monitoring
- mHealth Apps
- Teletherapy
- Telepharmacy
- Top Use Cases of Telemedicine Apps
- Some Common telemedicine apps in US
- Telemedicine regulations in the US
- Recommended Technology Stack for telemedicine application
- The future of Telemedicine apps
- AI and Machine Learning Integration
- Enhanced Remote Monitoring Capabilities
- Personalization and Adaptive Interfaces
- How Daffodil Can help?
-
A brief about telemedicine app development
Telemedicine app development is all about creating digital platforms that connect patients with healthcare providers through interactive technology. These apps enable virtual consultations, secure messaging, and easy access to medical records, making healthcare more accessible and convenient. With more than 100 successful healthcare software projects under our belt, Daffodil Software is your trusted guide and technology partner for telemedicine app development. We specialize in creating feature-loaded and user-friendly telemedicine applications that are customized to cater to your unique ideas or business requirements.
-
The Market Health of Telemedicine apps
The telemedicine app market has been booming and shows no signs of slowing down. Market research shows that in 2023, the market was valued at $87.21 billion and is projected to grow at an impressive compound annual growth rate (CAGR) of 19.3%, reaching a massive $426.90 billion by 2032.
Key drivers include the rising prevalence of chronic conditions, the convenience of virtual consultations, and significant investments in telehealth infrastructure. Consumers are embracing the idea of virtual consultations, with surveys indicating that nearly 75% of patients are willing to use telehealth services for follow-ups, and more than 60% prefer it for non-emergency situations.
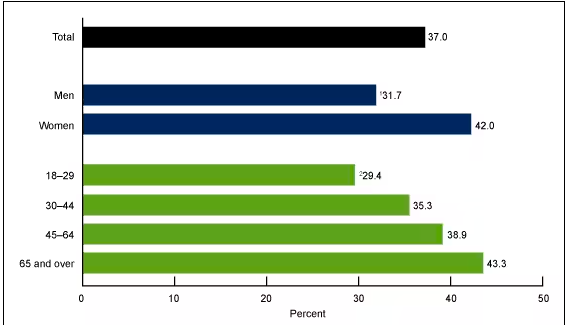
Percentage of adults in the United States who used telemedicine in the past 12 months, by sex and age.
Source: https://www.cdc.gov/nchs/products/databriefs/db445.htm
-
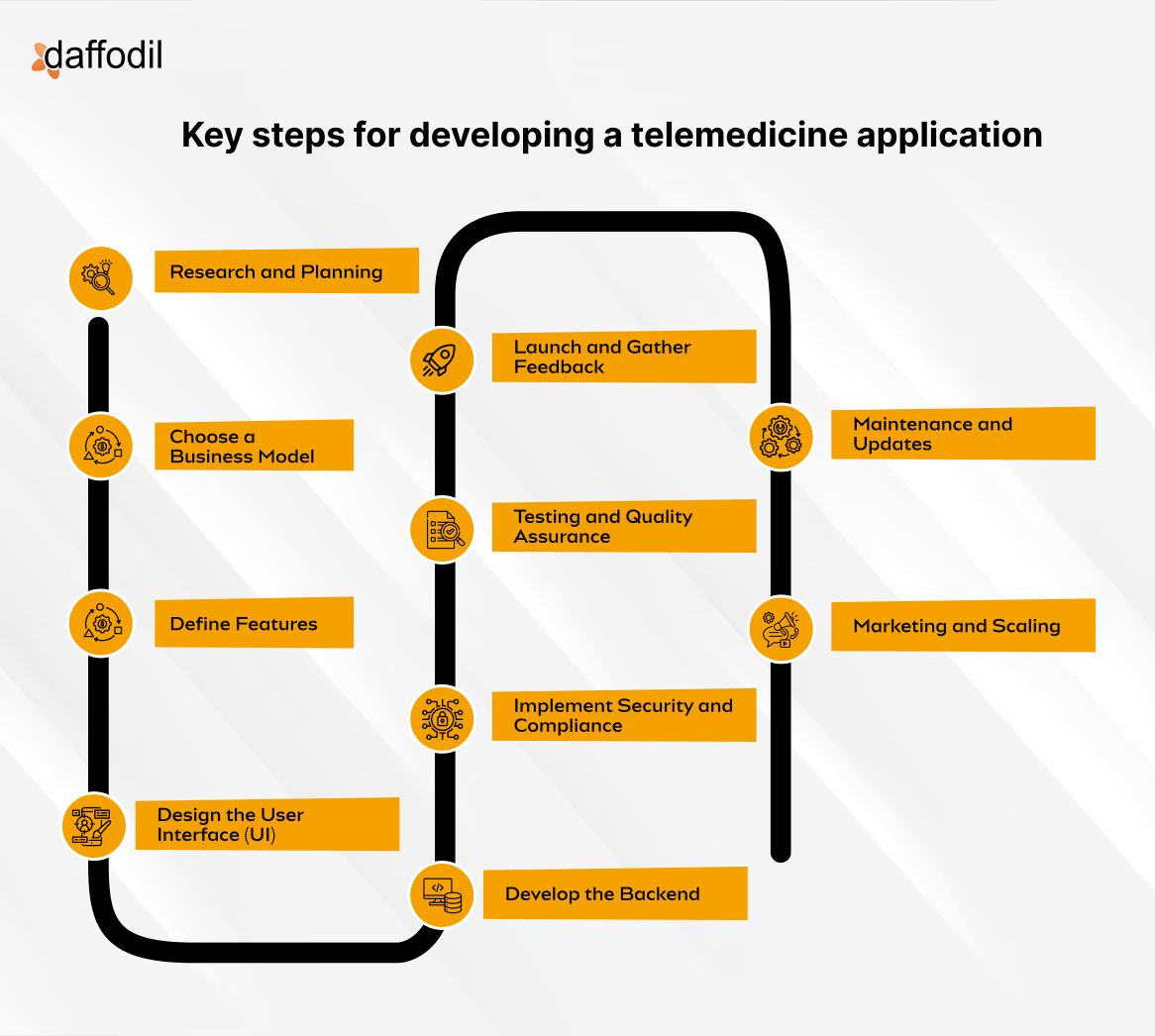
How to develop a telemedicine application?
Developing a telemedicine app requires careful planning, collaboration, and an understanding of both the healthcare industry and technology. Here’s a simple breakdown of the key steps:
-
1. Research and Planning
Start by researching the market, target audience, and regulations like HIPAA (for the U.S.) to ensure data security and compliance. This step is crucial to defining the scope of your project and understanding user needs, competition, and the legal landscape.
-
2. Choosing a Business Model
Decide how your app will generate revenue. Common models include subscription-based services, pay-per-visit, or partnerships with healthcare providers. Choose one that aligns with your target audience and long-term goals.
-
3. Define Features
Outline essential features, such as video conferencing, chat functionality, EHR/EMR integration, appointment scheduling, and payment processing. Consider adding optional features like AI-powered diagnosis or remote patient monitoring to differentiate your app.
-
4. Design the User Interface (UI)
Create a user-friendly design that makes it easy for both patients and doctors to navigate the app. The interface should be intuitive, especially for patients who may not be tech-savvy. Focus on clear layouts, easy access to important features, and a seamless user experience.
-
5. Develop the Backend
The backend is the engine that powers your app, ensuring smooth operations and data processing. It must be secure, scalable, and capable of handling sensitive medical data. Choose technologies that ensure security, performance, and compliance with healthcare standards.
-
6. Implement Security and Compliance
Since telemedicine apps handle sensitive patient data, strong encryption, secure authentication, and compliance with regulations (HIPAA in the U.S., GDPR in Europe) are critical. This ensures that patient information is protected from breaches.
-
7. Testing and Quality Assurance
Test your app thoroughly to identify bugs, ensure reliability, and check for potential security vulnerabilities. It’s important to simulate real-world scenarios with healthcare professionals and patients to ensure the app works smoothly in practice.
-
8. Launch and Gather Feedback
After a successful testing phase, launch the app. Start with a soft launch to gather feedback from early users. Based on this feedback, make necessary tweaks to improve user experience and performance.
-
9. Maintenance and Updates
Once the app is live, regular updates will be required to fix bugs, improve security, and add new features. Software maintenance and updates are essential to keep your app running smoothly and stay competitive.
-
10. Marketing and Scaling
Once your app is functional, create a marketing strategy to attract users. You can work with healthcare providers, advertise through digital channels, or offer free trials to gain traction. As you grow, ensure your infrastructure can scale to handle more users.
By following these steps, you’ll create a telemedicine app that not only serves patients efficiently but also meets all necessary compliance and security standards
-
How much does a telemedicine application cost?
The cost of developing a telemedicine application can vary significantly based on various factors such as the complexity of the app, the features included, the development team, and the technology stack. A typical telemedicine app can cost anywhere from $40,000 to $200,000 or more.
Let’s break down the costs into granular levels:
-
Type of Telemedicine App
The nature of the telemedicice app influences its overall cost. Apps can range from simple video consultation platforms to more advanced, comprehensive systems integrated with EHR (Electronic Health Records), remote monitoring devices, or AI-powered diagnostic tools. Below are the typical types:
- Basic Consultation Apps (e.g., video calls, messaging): $30,000–$100,000
- Advanced Telehealth Platforms (e.g., multi-user portals, EHR integration, health analytics): $100,000–$300,000+
- Telemedicine Platforms with IoT/AI Integration: $250,000–$500,000
-
Design Costs
UI/UX design is critical in creating a user-friendly experience. Design costs will depend on the complexity and customization of the app. This can involve:
- User Interface (UI) Design: Crafting intuitive, visually appealing interfaces for patients and healthcare providers.
- User Experience (UX) Design: Ensuring ease of use and smooth navigation.
Typical design costs range from $5,000 to $20,000 depending on complexity and number of screens.
-
Development Costs
App development is the largest expense and includes both frontend and backend development.
- Frontend Development: Focuses on what the user interacts with (e.g., video consultations, appointment scheduling). The cost for frontend development is around $20,000 to $70,000 depending on the number of features and supported platforms (iOS, Android, Web).
- Backend Development: The server-side infrastructure, including databases, APIs, and cloud storage to ensure secure communication and data processing. Backend costs generally range from $30,000 to $100,000+, especially if integrating complex features like AI-based recommendations or multi-device synchronization.
-
Features and Functionality
The number of features included has a direct impact on the cost of development. Some common features in telehealth apps and their estimated costs include:
- Video Conferencing: $10,000–$30,000
- Appointment Scheduling: $5,000–$10,000
- Patient/Provider Profiles: $2,000–$5,000
- EHR Integration: $10,000–$50,000+
- Remote Monitoring via IoT Devices: $20,000–$100,000+
- Payment Gateway Integration: $5,000–$15,000
- AI-based Diagnostics or Chatbots: $15,000–$60,000+
- HIPAA-Compliant Messaging: $10,000–$30,000
-
Third-Party Integrations
Many telehealth apps need to integrate with third-party systems such as:
- Electronic Health Record (EHR) Systems: This ensures patient data is accessible and updated.
- Pharmacy or Prescription APIs: To facilitate e-prescribing.
- Health Monitoring Devices: For IoT-based remote health monitoring.
- Payment Gateways: To allow patients to pay for consultations.
Each integration can cost $5,000 to $25,000 depending on the complexity and the number of third-party systems involved.
-
Compliance and Security
Since telehealth apps handle sensitive health data, complying with legal regulations such as HIPAA (in the US), GDPR (in Europe), or other healthcare regulations is crucial. Costs for ensuring compliance include:
- HIPAA Compliance Setup: $5,000–$25,000
- Data Encryption & Security Protocols: $3,000–$15,000
- Audit and Compliance Certification: $10,000–$30,000
-
Quality Assurance (QA) & Testing
Thorough testing is required to ensure the telehealth app functions properly across all devices and under different network conditions. This includes unit testing, load testing, and security testing. QA and testing costs are generally $10,000 to $30,000, depending on the complexity of the app.
-
Post-Launch Maintenance and Support
Once the app is launched, ongoing maintenance and updates are necessary to keep it running smoothly, resolve bugs, and add new features. This can include:
- App Updates and Bug Fixes: $5,000–$15,000 per year
- Server and Database Maintenance: $5,000–$20,000 per year
- Customer Support and Monitoring: $10,000–$30,000 per year
-
Cloud Infrastructure and Hosting
If your app involves video consultations, storing medical data, or remote monitoring, you will need cloud services to handle data storage and processing.
- Cloud Hosting (AWS, Google Cloud, Azure): $2,000–$10,000 per month, depending on the scale of the platform and the volume of data stored.
- Video Conferencing Bandwidth: Additional costs depending on the volume of video calls.
-
Marketing and Launch Costs
To ensure the telehealth app reaches its target audience, you’ll need to invest in marketing, which includes:
- App Store Optimization (ASO): $2,000–$5,000
- Digital Marketing Campaigns: $10,000–$50,000
-
What are different monetization models of tele-medicine applications?
1. Pay-Per-Visit
This is the simplest and most straightforward model. Patients pay for each consultation or visit they book through the app, just like a traditional in-person doctor’s visit. The telemedicine platform takes a percentage of the fee as a service charge, and the rest goes to the healthcare provider.
- Pros: Easy to understand for patients, quick revenue generation.
- Cons: Revenue is inconsistent since it depends on how often people use the app.
2. Subscription Plans
Instead of charging per visit, you can offer subscription-based access. Patients pay a monthly or yearly fee to get unlimited or discounted consultations within a given period.
- Pros: Predictable, recurring revenue; encourages long-term use.
- Cons: People need to see value in the subscription, or they’ll cancel—especially if they’re not sick often!
3. Freemium Model
The freemium model gives patients access to basic features for free, while charging for premium features like specialist consultations, extended video calls, or AI-driven health analytics. It’s a great way to attract a large user base, and once they’re hooked on the free stuff, you can upsell them.
- Pros: Attracts a lot of users; potential for high conversion to paid services.
- Cons: You need to strike a balance between what’s free and what’s premium, or users may never feel the need to upgrade.
4. Commission-Based
This model involves charging healthcare providers a commission for each consultation or service provided through the app. It’s similar to the pay-per-visit model but shifts the burden of payment to the healthcare professionals rather than the patients.
- Pros: Revenue grows as the platform attracts more healthcare providers.
- Cons: Providers might push back against commission fees if they feel the app isn’t providing enough value.
5. Partnership with Insurance Providers
Partnering with insurance companies can open up another revenue stream. You negotiate with insurance providers to cover telemedicine consultations, allowing patients to pay using their insurance. You get paid by the insurance company directly.
- Pros: Insurance makes healthcare more accessible, increasing app usage.
- Cons: Dealing with insurance companies can be slow and bureaucratic, plus it can complicate your pricing model.
6. Advertisement
This is more of a complementary monetization model. You can allow healthcare-related companies (pharmaceuticals, health product manufacturers, etc.) to advertise on your app. You could display banners, video ads, or even sponsored content.
- Pros: Doesn’t affect the user’s wallet; additional income stream.
- Cons: Ads can be intrusive, and if not done tastefully, they can frustrate users. Also, it’s not the most reliable source of income unless you have a huge user base.
7. Selling Medical Products
Integrating an eCommerce section where users can buy medications, health monitoring devices, supplements, or other healthcare products is a natural fit for telemedicine apps. You could take a commission on sales or partner with a pharmacy or medical device provider.
- Pros: Easy upsell opportunity for users who are already consulting doctors and may need medications or devices.
- Cons: You’ll need to handle logistics like inventory, shipping, and customer service if you manage this in-house.
8. White-Labeling and Licensing
Another lucrative option is to white-label your telemedicine platform and license it to hospitals, clinics, or even insurance companies who want their own telemedicine apps but don’t want to build one from scratch.
- Pros: High revenue potential with minimal ongoing maintenance.
- Cons: Customizing the app for each client might require significant upfront work.
9. Data Monetization (Ethically!)
With a ton of user data (of course, anonymized and aggregated), you can sell insights to pharmaceutical companies, healthcare research firms, or governments to help them understand health trends. But, and this is a big but, you have to be extra careful with patient privacy and data security. Think HIPAA compliance and GDPR regulations!
- Pros: High-value data can bring in significant revenue.
- Cons: Ethical and regulatory hurdles. If not done properly, it can damage trust in your platform.
It depends on your app’s target audience, the types of services offered, and your long-term goals. Often, a combination of these models works best—like offering a freemium model to attract users, along with subscription plans for power users, and ads for extra revenue. The key is to create a system that delivers value to both patients and healthcare providers while making your platform profitable.
-
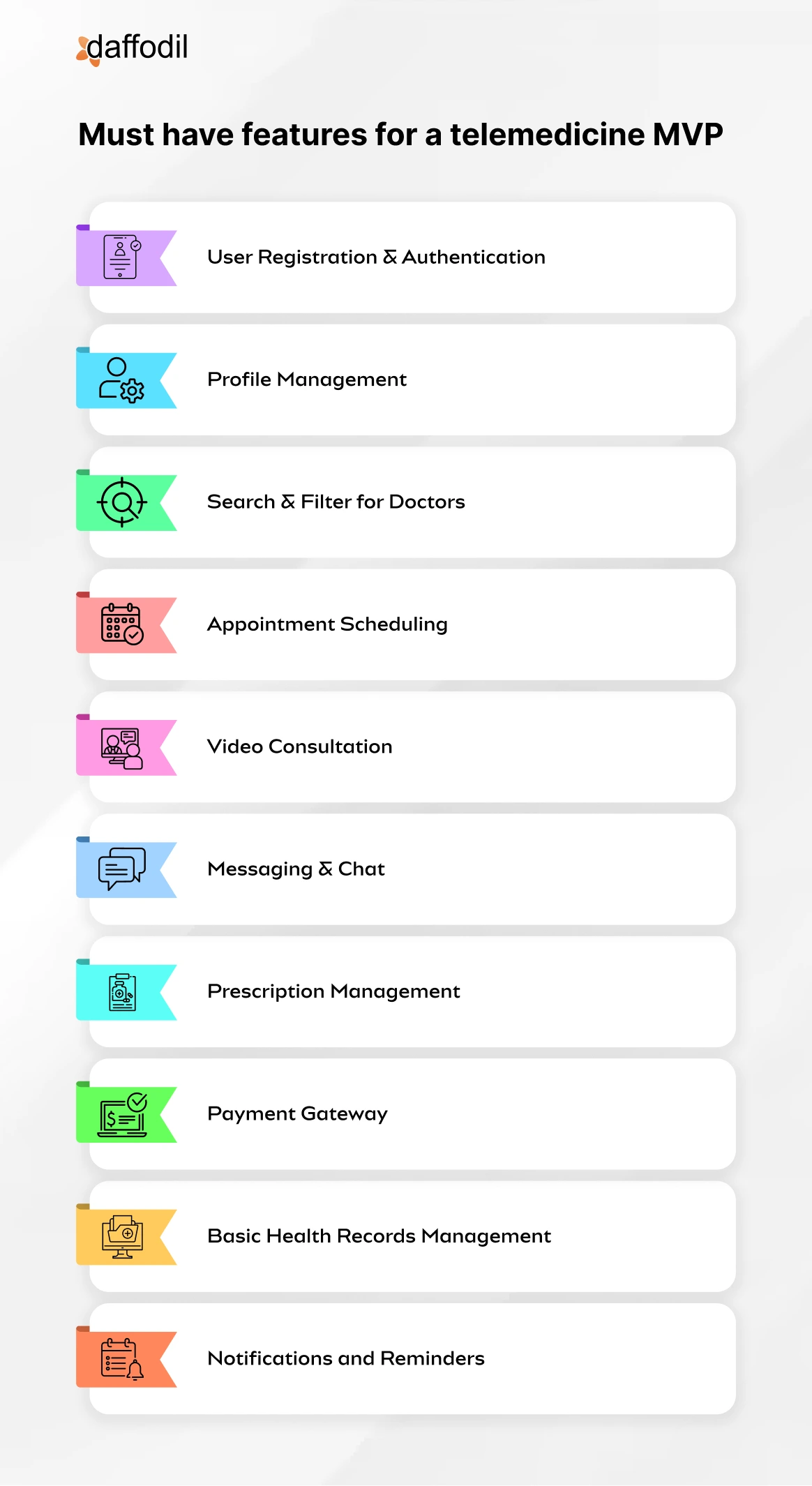
Essential features that a telemedicine MVP should have
If you’re building a telemedicine app, the key is starting with a Minimum Viable Product (MVP)—something that gets you into the market fast with just enough features to be functional and valuable, without going overboard. Here’s a list of essential features your telemedicine MVP should have, and why they matter:
1. User Registration & Authentication
This is your basic entry point for both patients and healthcare providers. Secure logins (email, phone, or social sign-ons) ensure that sensitive data stays safe, and users can access the platform easily.
2. Profile Management
Both patients and doctors need profiles. Patients need to store personal health information, and providers need professional profiles so patients can trust them. Keep it simple—name, contact info, health history for patients; certifications, specialties, and availability for doctors.
3. Search & Filter for Doctors
Patients need to quickly find the right specialist. A basic search with filters (e.g., specialty, language, location, availability) makes the process easy and convenient.
4. Appointment Scheduling
No one wants to play email tag to schedule appointments. Let patients book an appointment directly from the app. Sync with doctors’ calendars to show available slots, and offer options for both instant and future consultations.
5. Video Consultation
Why it’s required: This is the core feature of any telemedicine app. Integrate a stable, HIPAA-compliant video conferencing solution. It doesn’t need to be fancy—just reliable and clear. Make sure you allow both one-on-one video calls and group consultations for when family members need to join.
6. Messaging & Chat
Sometimes patients have follow-up questions that don’t require a video call. Secure, HIPAA-compliant messaging is a must for simple, quick communication between doctor and patient.
7. Prescription Management
After the consultation, doctors need to be able to prescribe medications. A basic e-prescription feature helps the doctor send prescriptions digitally and securely to the patient or directly to their pharmacy.
8. Payment Gateway
Integrate a simple payment system so patients can pay for their consultations via credit card, PayPal, or other payment options. Make it frictionless to avoid cart abandonment. Plus, this ensures you can start generating revenue right away.
9. Basic Health Records Management
Let patients upload and store important health records (like lab results, previous prescriptions, etc.) in their profile. This helps doctors have all the context they need during consultations. Don’t overcomplicate this at first—just basic file storage will do for an MVP.
10. Notifications and Reminders
People forget. Simple push notifications or SMS reminders for upcoming appointments, new messages, or prescription refills help keep the patient engaged and the app relevant.
Nice-to-Have, but Optional for MVP
Here are some features that are cool to have but not essential for your MVP:
- Remote Patient Monitoring: Collecting data from wearable devices and integrating it into the app. Useful, but not necessary for the initial launch.
- AI-Based Symptom Checkers: It’s trendy but complex. You can add this in the next phase after you get your basic product out
Watch the video: How we developed a custom telehealth application for a US-based mental healthcare service provider
-
Essential features that a full-fledged application should have
Once you’ve gone beyond the MVP stage and your telemedicine app is gaining traction, it’s time to step up your game and add the features that make your app stand out. A full-fledged telemedicine platform needs to offer more than just basic video consultations and appointment scheduling. Here’s a list of the must-have features for a fully developed telemedicine app:
1. Comprehensive User Profiles
You’ll want to expand patient and provider profiles. For patients, this could include detailed health records, allergy information, ongoing treatments, and medical history. For providers, verified certifications, availability, and ratings from past consultations should be displayed. This builds trust and ensures doctors have the necessary context for consultations.
2. Advanced Appointment Scheduling
This includes setting recurring appointments, sending automatic reminders, syncing with personal calendars, and even offering a virtual waiting room for patients waiting to connect with a doctor. Flexibility is key.
3. Multi-Device Accessibility
Your app should work seamlessly across all devices—smartphones, tablets, desktops, and wearables. This allows patients and doctors to access the platform from anywhere, enhancing convenience.
4. Integrated EHR/EMR (Electronic Health Records)
Integrating an Electronic Health Record (EHR) or Electronic Medical Record (EMR) system is crucial. It allows healthcare providers to access and update patient records in real-time. Patients can also share their medical records with other providers easily. This ensures continuity of care and helps avoid misdiagnosis or treatment errors.
5. AI-Powered Symptom Checker
Adding an AI-based symptom checker lets patients input their symptoms and get preliminary advice on potential conditions or whether they need to schedule a consultation. It helps triage patients more effectively and offers them a quicker solution to their problems.
A must-read success story: See how we developed an AI-based symptom-tracking application for MayaMD.
6. Remote Patient Monitoring
For chronic patients or those with ongoing treatments, integrating remote patient monitoring via wearables or IoT devices is a game-changer. Data like blood pressure, glucose levels, heart rate, etc., can be collected and analyzed in real-time, allowing doctors to provide proactive care.
7. Multiple Consultation Types
Offer different consultation options—audio-only calls, chat-based consultations, or video calls. Some patients may prefer to speak without video, while others might just need a quick chat without setting up a full video session.
8. Group Consultations
In cases where family members or multiple healthcare providers need to be present, group consultations make it easier to facilitate multi-party discussions about a patient’s treatment plan. It’s also helpful for second opinions or family check-ins.
9. In-App Pharmacy & Prescription Fulfillment
Make the process easy for patients by integrating an in-app pharmacy. After the consultation, patients can have their prescriptions filled directly from the app, either by home delivery or for pickup at a nearby pharmacy. This convenience can boost patient satisfaction and streamline the entire experience.
10. In-App Billing & Insurance Integration
Beyond simple payment gateways, a full-fledged app should offer insurance integration, allowing patients to pay for consultations through their health insurance plans. The app should also support direct billing, co-pays, and the ability to submit claims automatically.
11. Specialist Referrals
Often, a general practitioner may need to refer a patient to a specialist. Your app should allow for referrals and even book the appointment with the specialist within the platform. The patient’s medical records should be automatically shared with the referred doctor to avoid duplicate tests or assessments.
12. Health Education Resources
Offer patients educational content like articles, videos, and webinars related to health conditions, treatment plans, and wellness tips. This adds value for the patient and keeps them engaged with your app even when they’re not actively using it for consultations.
13. HIPAA and GDPR Compliance
Ensuring data privacy is non-negotiable in telemedicine. Your platform must be fully compliant with HIPAA (in the US) and GDPR (in Europe) to ensure patient data is encrypted, protected, and handled ethically. This includes secure video calls, encrypted messaging, and strict access controls for medical records.
14. Doctor & Patient Ratings and Reviews
Having a rating and review system builds trust in the platform. Patients can rate their experience with doctors, and doctors can leave feedback on patients. It helps the app maintain a quality standard while allowing users to make informed choices.
15. Admin Dashboard & Analytics
For platform owners, having an admin dashboard is crucial for monitoring user activity, appointment volume, revenue, and overall app performance. Analytics can also help identify patterns like peak consultation hours, user behavior trends, and popular specializations, which can inform future upgrades and marketing strategies.
16. Emergency Services Integration
Allow patients to access emergency services within the app, like instant connections to 911 or other emergency medical services. This feature can be a lifesaver (literally) for patients needing urgent medical attention.
17. Customizable Notifications & Reminders
Go beyond the basics of appointment reminders. Include customizable notifications for things like prescription renewals, follow-up consultations, or health tips based on a patient’s history.
18. Teletherapy & Mental Health Support
Expand your offerings to include teletherapy or mental health consultations. You can also opt for a custom mental health app development. This is a booming sector of telemedicine, and adding licensed therapists or mental health professionals can broaden your app’s appeal.
19. Multi-Payment Options
Some patients may prefer credit cards, others may want to use digital wallets or health savings accounts. Offering a variety of payment options (even cryptocurrency, in some cases) can make transactions smoother and reduce friction in the checkout process.
-
Breaking Down the Types of Telemedicine applications
Telemedicine has been around in various forms for years, but it truly skyrocketed during the pandemic, allowing patients to connect with healthcare providers without leaving their homes. But telemedicine isn’t one-size-fits-all. Let’s break down some key types, each with its unique benefits and use cases.
-
Real-time Telemedicine (Synchronous Telemedicine)
Real-time telemedicine is all about those live video calls with your healthcare provider. Whether you’re chatting through a video platform or on the phone, it’s immediate, interactive, and feels pretty close to an in-person visit.
This type works well for consultations, urgent care, mental health check-ins, or even post-operative follow-ups. It’s especially helpful for people with limited mobility, those who live in remote areas, or anyone who’s pressed for time.
-
Store-and-Forward Telemedicine (Asynchronous Telemedicine)
Store-and-forward telemedicine is the behind-the-scenes version of telemedicine. You don’t need to be on a live call with your provider for this one. Instead, you send over your medical data, like X-rays, images, or reports, for the provider to review at their convenience. Dermatologists, radiologists, and pathologists use this a lot, as it allows them to take their time analyzing and getting back to patients when ready. It’s all about convenience without the rush of real-time interactions.
-
Remote Patient Monitoring
Remote Patient Monitoring, or RPM, takes telemedicine a step further by continuously tracking patients’ health data. It’s perfect for chronic conditions like diabetes, hypertension, or heart issues. Patients wear devices (think blood pressure cuffs, glucose monitors, etc.) that automatically send data to their healthcare team. RPM allows for a proactive approach where doctors can catch early signs of potential problems before they escalate. It gives patients peace of mind knowing they’re being monitored around the clock.
-
mHealth Apps
mHealth is essentially the telemedicine that lives in your pocket. It’s all those health-related apps on your phone that track things like your steps, heart rate, diet, or sleep patterns. mHealth also covers SMS reminders, telehealth portals, and medication tracking apps. It empowers patients to take control of their health in the easiest way possible—through their mobile devices.
-
Teletherapy
Teletherapy is where mental health meets telemedicine. Therapy sessions have successfully gone virtual, offering patients a more flexible way to access mental health support. Video sessions work well, but even phone calls or texting services can make a difference. It’s ideal for people who might feel hesitant about traditional therapy, those with a tight schedule, or people who simply feel more comfortable chatting from home.
-
Telepharmacy
Telepharmacy takes the pharmacy online, connecting patients with pharmacists through a screen rather than at a counter. Patients can discuss their medications, potential side effects, or dosing questions from wherever they are. Telepharmacy works particularly well for rural areas without local pharmacies, offering convenient and accessible support without extra travel.
Telemedicine is transforming how we think about healthcare. With options that cater to different needs, telemedicine makes it easier for patients to manage their health on their own terms. Whether it’s live, on-demand, or monitoring in the background, there’s a telemedicine solution for almost everyone.
-
Top Use Cases of Telemedicine Apps
From virtual consultations to chronic disease management, telehealth apps provide a range of services that save time and improve patient care. Here are the top use cases where telemedicine apps are making a significant impact.
1. Virtual Consultations
- Consult doctors via video or voice calls.
- No need to travel or sit in waiting rooms.
- Ideal for routine checkups, follow-ups, and non-emergency advice.
2. Chronic Disease Management
- Regular check-ins and monitoring for conditions like diabetes, hypertension, and asthma.
- Personalized treatment plans via the app.
- Helps patients manage conditions without frequent clinic visits.
3. Mental Health Support
- Connect with therapists and counselors through video or chat sessions.
- Provides privacy and convenience for mental health care.
- Increases access to mental health services for people who might not seek in-person help.
4. Post-Surgery Follow-ups
- Patients can have follow-up appointments through video calls.
- Easily track recovery progress and get advice from surgeons.
- Reduces the need for post-surgery trips to the hospital.
5. Prescription Refills
- Quick and easy way to consult with doctors for prescription renewals.
- Saves time by eliminating the need for in-person doctor visits.
- Patients can manage regular medications conveniently.
6. Remote Monitoring
- Uses wearables and connected devices to monitor patient health in real-time.
- Alerts doctors to any anomalies for quick intervention.
- Particularly useful for chronic conditions like heart disease and diabetes.
7. Specialist Consultations
- Access specialists from other cities or countries without traveling.
- Reduces wait times for specialized care.
- Improves treatment outcomes, especially for rare or complex conditions.
8. Second Opinions
- Easily share medical records with multiple doctors for second opinions.
- Helps patients make informed decisions about their health.
- Convenient for those facing major treatment decisions or complex diagnoses.
9. Preventative Care and Education
- Offers wellness tracking and educational tools to promote healthy habits.
- Includes dietary advice, exercise plans, and preventative care measures.
- Empowers patients to maintain better health and avoid medical issues.
-
Common telemedicine apps in US
Several applications have emerged as frontrunners, offering innovative solutions for patients and healthcare providers alike. Here’s a look at some of the leading telemedicine apps in the United States:
1. Teladoc Health
Overview: Teladoc is one of the largest telemedicine platforms in the US, providing on-demand virtual healthcare services across various specialties.
Key Features:
- Comprehensive Services: Offers services for both urgent care and chronic condition management.
- 24/7 Availability: Accessible at any time, allowing patients to connect with doctors whenever needed.
- Personalized Care: Utilizes advanced technology to tailor healthcare advice based on individual patient needs.
Why It Stands Out: Teladoc’s extensive network of licensed physicians ensures patients receive timely and reliable care, making it a top choice for many.
2. Zocdoc
Overview: While Zocdoc started as a scheduling platform, it has evolved to include telemedicine services for numerous health specialties.
Key Features:
- Find Providers Easily: Patients can search for telehealth appointments across various specialties.
- Real-Time Availability: Patients can see which doctors have immediate openings for telehealth consultations.
- Verified Patient Reviews: Offers a robust review system to help patients make informed decisions.
Why It Stands Out: Zocdoc combines appointment scheduling and telemedicine effectively, ensuring users can find the right care at the right time.
Also read: How Zocdoc Works? Business Model and Revenue Streams
2. Amwell
Overview: Amwell connects patients with board-certified doctors for virtual visits, focusing on urgent care and behavioral health.
Key Features:
- Specialty Services: Availability of various specialties, including psychiatry and nutrition counseling.
- Insurance Partnerships: Works with multiple insurance providers, facilitating payments and minimizing out-of-pocket costs.
- User-Friendly Interface: Simple navigation makes it easy for users of all ages to access healthcare.
Why It Stands Out: Amwell’s focus on convenience and its robust network of specialists make it an appealing option for comprehensive telehealth services.
3. MDLive
Overview: MDLive offers an easy-to-use platform for users seeking virtual consultations with healthcare professionals.
Key Features:
- Wide Range of Care: Specializes in urgent care, dermatology, and behavioral health, providing a holistic approach to patient care.
- Express Healthcare: Patients can go through a quick process to get prescriptions for common illnesses.
- Mobile App Accessibility: Strong mobile app support allows patients to schedule appointments and consult providers on-the-go.
Why It Stands Out: MDLive combines speed with quality, ensuring patients receive prompt care while maintaining high standards of service.
5. HealthTap
Overview: HealthTap allows patients to ask health questions and get real-time answers from licensed doctors.
Key Features:
- AI-Powered Symptom Checker: Uses artificial intelligence to help patients understand potential conditions based on their symptoms.
- Text-Based Chat Options: Patients can consult doctors via text, allowing for more straightforward communication.
- Personalized Health Profiles: Users can create profiles for tailored healthcare experiences.
Why It Stands Out: HealthTap integrates technology with healthcare, providing patients with immediate information and bridging the gap for easy communication.
-
Telemedicine regulations in the US
Practitioner Requirements
- Most states expect providers to hold a license where the patient lives.
- Some states make it easier with interstate compacts like the Interstate Medical Licensure Compact (IMLC).
- An initial in-person visit is often needed before telemedicine kicks in, though this varies a lot.
Prescription Rules
- For controlled substances, an in-person evaluation is generally non-negotiable (thanks to the federal Ryan Haight Act).
- Some states go further, restricting certain meds via telemedicine.
- COVID-19 brought temporary leniency in prescription rules, but whether those changes stuck around depends on the state.
Technology Standards
- HIPAA-compliant platforms are the norm for video visits.
- Audio-only visits are allowed in some states, but restricted in others.
- Store-and-forward (asynchronous) telemedicine has varying levels of acceptance
Documentation & Consent
- Nearly all states require documented patient consent for telemedicine services
- Medical records requirements generally mirror in-person visit standards
- Many states require patients to be informed about telemedicine limitations and alternatives.
Insurance Coverage
- Most states have some form of telehealth parity law requiring insurance coverage Coverage requirements vary for different types of services (video vs. audio-only)
- Reimbursement rates and covered services differ significantly by states
A Few State-Specific examples:
- California: Patients must be informed about privacy risks and give consent. Non-controlled substances can be prescribed via telemedicine after a provider-patient relationship is established.
- Texas: Physician-patient relationships can be formed through telemedicine, but synchronous (live) audiovisual interactions are typically required for first visits, with some exceptions.
- Florida: Telehealth prescribing has strict rules, like documenting the rationale for remote prescriptions. Providers must either be licensed in Florida or register as out-of-state practitioners.
-
Recommended Technology Stack for telemedicine application
A well-designed telemedicine application relies on a robust and diverse technology stack to ensure functionality, security, scalability, and a seamless user experience. The technology stack of a telemedicine platform typically includes the following components:
1. Frontend Technologies
The frontend or user interface is where patients, doctors, and healthcare providers interact with the system. It needs to be intuitive, responsive, and accessible across devices.
- Web Technologies: HTML5, CSS3, and JavaScript frameworks like React.js, Vue.js, or Angular are commonly used for building web-based telemedicine apps. These frameworks allow for dynamic, user-friendly interfaces that function well across different devices and screen sizes.
- Mobile Technologies: For mobile applications, Swift (for iOS) and Kotlin or Java (for Android) are the primary languages used. Alternatively, cross-platform frameworks like Flutter or React Native are also popular for developing applications that work seamlessly on both iOS and Android devices.
2. Backend Technologies
The backend is the powerhouse of a telemedicine application, handling data storage, business logic, and user authentication.
- Programming Languages: Popular backend languages include Node.js, Python (Django/Flask), Ruby on Rails, Java (Spring Boot), and PHP (Laravel). These frameworks are chosen based on the application’s specific needs and the development team’s expertise.
- APIs: A telemedicine application often integrates with third-party services via RESTful or GraphQL APIs. These might include EHR/EMR systems, appointment scheduling systems, and billing platforms.
- Database: Databases are critical for storing patient data, appointment histories, prescriptions, etc. Popular options include PostgreSQL, MySQL, and MongoDB. NoSQL databases like Firebase may be used for real-time data needs such as chat systems.
- Real-Time Communication: To enable real-time video consultations, chat, and file sharing, WebRTC is widely used for peer-to-peer connections. Socket.io or Firebase can also manage real-time data for chat or notifications.
3. Cloud and DevOps
Scalability and uptime are essential for telemedicine apps to handle varying loads and maintain high availability.
- Cloud Providers: Amazon Web Services (AWS), Microsoft Azure, and Google Cloud Platform (GCP) are popular choices for hosting and scaling telemedicine applications. They offer solutions like Elastic Compute Cloud (EC2) for computing power, S3 or Blob Storage for file storage, and RDS or Cloud SQL for databases.
- Containerization: Tools like Docker and orchestration platforms like Kubernetes enable scalable deployments by packaging applications into containers and managing their lifecycle.
- CI/CD Pipelines: Jenkins, CircleCI, and GitLab CI are commonly used to automate continuous integration and deployment (CI/CD) to ensure the application can be updated frequently without downtime.
4. Security and Compliance
Security is paramount in telemedicine applications to protect sensitive patient data and ensure regulatory compliance. Our healthcare compliance consulting services can help you achieve just that.
- Data Encryption: End-to-end encryption, both at rest and in transit, is crucial. Protocols like SSL/TLS for web security and AES for data encryption are commonly used.
- HIPAA Compliance: For telemedicine apps used in the U.S., the backend must be compliant with HIPAA (Health Insurance Portability and Accountability Act). This involves secure data storage, access controls, audit logs, and ensuring third-party services also meet HIPAA standards.
- Authentication: Secure authentication mechanisms such as OAuth2.0, JWT (JSON Web Tokens), or Multi-factor Authentication (MFA) are used to ensure secure user access.
5. AI and Machine Learning
Artificial Intelligence and Machine Learning play an increasingly important role in telemedicine to enhance diagnosis, offer personalized healthcare, and improve user engagement.
- Natural Language Processing (NLP): Tools like Google NLP or IBM Watson are integrated to enable features like symptom checkers or medical chatbots that can interact with patients conversationally.
- Predictive Analytics: AI-driven algorithms can predict patient outcomes, recommend treatment options, or assist healthcare providers in making informed decisions based on patient data.
Watch related success story: Developing an AI-integrated symptom tracking application for MayaMD.
6. Third-Party Integrations
- Electronic Health Records (EHRs)/EMRs: Telemedicine apps often integrate with popular EHR/EMR platforms like Epic, Cerner, or AthenaHealth to access patient records, medical history, and lab results.
- Payment Gateways: Stripe, PayPal, or Square are typically integrated to handle payments for telemedicine consultations or services.
- Pharmacy Integration: To enable e-prescriptions, telemedicine apps often integrate with pharmacies or e-pharmacy platforms such as CVS or Walgreens.
7. Monitoring and Analytics
Continuous monitoring is crucial to ensure uptime and performance.
- Monitoring Tools: Tools like Prometheus, Grafana, New Relic, or Datadog help monitor the application’s performance, detect anomalies, and prevent downtime.
- Analytics: Integration with analytics platforms like Google Analytics, Mixpanel, or Amplitude helps track user engagement and system usage to improve service quality.
8. Technical Architecture Considerations
- Cloud vs. On-Premises Hosting OptionsCloud hosting offers scalability, reduced maintenance burden, and pay-as-you-go economics ideal for growing telemedicine platforms. On-premises solutions provide maximum control over sensitive patient data and may be preferred for stringent compliance requirements. Hybrid approaches can leverage cloud flexibility while keeping critical PHI under direct control.
- Security Architecture Best PracticesImplement defense-in-depth strategies with multiple security layers including network segmentation, robust authentication mechanisms, and comprehensive encryption. Deploy Web Application Firewalls (WAF) alongside intrusion detection systems. Regular penetration testing and security audits should be mandatory. Consider Zero Trust architecture to minimize potential breach impact.
- Scalability Planning and InfrastructureDesign your architecture for elastic scalability from day one, allowing seamless handling of patient surges during health crises. Implement containerization with Kubernetes for dynamic resource allocation. Consider microservices architecture over monolithic systems to enable independent scaling of high-demand components like video consultation services.
- Data Storage and Management SolutionsImplement HIPAA-compliant database solutions with robust encryption for protected health information. Consider FHIR-compatible data models to facilitate interoperability. Separate operational data from analytical systems using ETL pipelines. Implement comprehensive data lifecycle policies including retention, archiving, and secure destruction protocols that align with healthcare regulations.
ALSO READ: How Daffodil developed an AI-powered telehealth application for a US-based health tech firm
-
The future of Telemedicine apps
The ecosystem of telemedicine apps is rapidly evolving due to technological advancements and changing healthcare needs. The following section explores key trends shaping telemedicine app development in the coming years.
-
AI and Machine Learning Integration
Automated Triage and Symptom Assessment
Advanced AI algorithms will conduct initial patient screenings, analyzing symptoms and medical history to determine urgency and recommended care paths. These systems will become increasingly sophisticated at identifying patterns and potential diagnoses, helping to streamline the healthcare process.
Predictive Analytics
Machine learning models will analyze patient data to predict health trends and potential complications before they become severe. This proactive approach will enable earlier interventions and better health outcomes.
Natural Language Processing
Improved NLP capabilities will enable more natural conversations between patients and virtual health assistants, making the experience more intuitive and accessible for users of all technical backgrounds.
-
Enhanced Remote Monitoring Capabilities
IoT Device Integration
Telemedicine apps will seamlessly integrate with an expanding ecosystem of IoT healthcare devices, including:
- Smart watches and fitness tracking apps
- Continuous glucose monitors
- Blood pressure monitors
- Sleep tracking devices
- Smart scales
This integration will provide healthcare providers with real-time patient data and enable more accurate remote diagnoses.
Advanced Biosensors
New generations of biosensors will expand the range of vital signs and health metrics that can be monitored remotely, including:
- Blood oxygen levels
- Respiratory rates
- Heart rhythm abnormalities
- Stress levels
- Medication adherence
-
Personalization and Adaptive Interfaces
Apps will automatically adjust their interfaces and functionality based on:
- User age and technical proficiency
- Physical capabilities and limitations
- Language preferences
- Cultural considerations
- Medical conditions
-
How Daffodil Can help?